Synopsis :
Definition
History and epidemiology
Aetiopathogenesis
Clinical features
Classification
DD
Management
Prognosis
Introduction :
Papulosquamous inflammatory disorder characterized by
Affect skin, mucous membrane, nail and hair
Prototype of lichenoid eruption
Lichen = tree moss Planus = flat
LP – name given by Erasmus Wilson in 1869
Whitish striae and punctation on flat LP lesion described by Wikham in 1895
Histological findings elaborated by Darier in 1909
Epidemiology :
Worldwide distribution
No racial predisposition
Less than 1% of general population affected
Age
Male – earlier
Female – late
Extremes of age – less common
Aetiopathogenesis :
Immunologically mediated disease in genetically susceptible individual
Other association –
Cutaneous LP - Hepatitis C, Anxiety and depression
Oral LP - Mercury and Gold sensitization
Clinical Features :
Shiny, violaceous, flat topped, polygonal, pruritic papules with ‘wickham striae’ and koebnerization
Insidious onset and size ranges from pinpoint to centimeters
Koebnerization
Wickhams striae
Affect Volar aspect of wrists, ankles, lumbar region with bilateral symmetrical distribution
Oral mucous membrane and genitalia are additional site of involvement
Pruritus - mild irritation to intolerable
Pinkish papule change to violaceous then to brown macule as disease progress
Variant of LP
Configuration
Site of involvement
Diagnosis
Clinical feature
Histology
Histology
Compact orthokeratosis
Wedge shaped hypergranulosis
Irregular acanthosis
Vacuolar alteration of the basal layer
Band like dermal lymphocytic infiltrates
Colloid bodies
Max –Joseph spaces
Management of LP
Challenging for both patient and physician
Only minor symptoms or considerable discomfort and disability
Many drugs lack conclusive evidence for efficacy
Oral LP
General measure
Good oral hygiene and regular professional dental care
Offending drugs or dental amalgam, gold- withdrawal and replacement
Topical lidocaine gel or Diphenhydramine for pain relief
Systemic Glucocorticoids
For extensive, ulcerative/erosive lesion of oral and vulvovaginal LP
Used alone or in conjunction with topical therapy
Prednisolone 30-80mg/day tapered over 3-6 weeks
Relapse after dose reduction or discontinuation
Retinoids
Topical tretinoin gel for erosive and plaque like lesion – less attractive because of irritation
Isotretinoin gel for nonerosive oral lesion-improves in 2 months-recovers after discontinuation
In conjunction with topical steroid
Acitretin 30mg/day complete remission in 8 weeks
Topical – beneficial but not available commercially
Miscellaneous
Griseofulvin – used empirically
Fluconazole, itraconazole – for candidal overgrowth, concomitant use with systemic steroid
Hydroxychloroquine – 200-400mg/d for 6 months – complete healing of oral lesion
Azathioprine, cyclophosphamide
Laser therapy
Surgical excision of persistent ulcer
Cutaneous LP
Potent creams is sufficient for symptomatic relief for small area, larger area needs dilution
Hypertrophic LP:-10-20mg/ml
Monitor for atrophy or hypopigmentation
Antihistamines for itching
Retinoids :
Acitretin : 30 mg / day for 8 weeks
Tretinoin : 10-30 mg/d
Etretinate : 10-20 mg/d
Photochemotherapy :
PUVA in generalized cutaneous LP
50 mg of Trioxsalen in 150 L of water - 10 min of UVA bath
75 patients – 65% cured ; 15% improved
Immunosuppressive therapy
Cyclosporine: 3-10 mg/kg/d
Azathioprine , mycophenolate mofetil
Ind : recalcitrant LP
Miscellaneous :
Dapsone : 200 mg/d
Hydroxychloroquine : 200-400 mg/d
IFN- α2b
Metronidazole : 500 mg b.d
Cyclophosphomide ,methotrexate
Prognosis :
Unpredictable ; 1-2 yrs
Duration α extent /site/ morphology
L planopilaris : most chronic
Generalised : rapid course
Gen < skin
Relapse : 15 -20 %
Definition
History and epidemiology
Aetiopathogenesis
Clinical features
Classification
DD
Management
Prognosis
Introduction :
Papulosquamous inflammatory disorder characterized by
- Distinctive color - Violacious
- Morphology – Flat topped papule
- Typical Location – Volar aspect of extremities
- Characteristic pattern of evolution
Affect skin, mucous membrane, nail and hair
Prototype of lichenoid eruption
History :
LP – name given by Erasmus Wilson in 1869
Whitish striae and punctation on flat LP lesion described by Wikham in 1895
Histological findings elaborated by Darier in 1909
Epidemiology :
Worldwide distribution
No racial predisposition
Less than 1% of general population affected
Age
Male – earlier
Female – late
Extremes of age – less common
Aetiopathogenesis :
Immunologically mediated disease in genetically susceptible individual
Other association –
Cutaneous LP - Hepatitis C, Anxiety and depression
Oral LP - Mercury and Gold sensitization
Clinical Features :
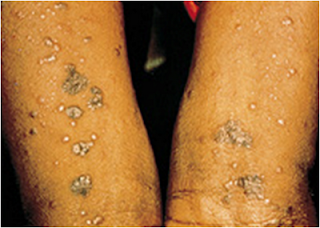
Shiny, violaceous, flat topped, polygonal, pruritic papules with ‘wickham striae’ and koebnerization
Insidious onset and size ranges from pinpoint to centimeters
Koebnerization
Wickhams striae
Affect Volar aspect of wrists, ankles, lumbar region with bilateral symmetrical distribution
Oral mucous membrane and genitalia are additional site of involvement
Pruritus - mild irritation to intolerable
Pinkish papule change to violaceous then to brown macule as disease progress
Variant of LP
Configuration
- Annular
- Linear
Site of involvement
- Palm and sole
- Mucous membrane
- Nail
- Scalp
Morphology of lesion
- Hypertrophic
- Atrophic
- Vesicobullous
- Erosive and Ulcerative
- Follicular
- Actinic
- Lichen Planus Pigmentosus
- Others
Diagnosis
Clinical feature
Histology
Histology
Compact orthokeratosis
Wedge shaped hypergranulosis
Irregular acanthosis
Vacuolar alteration of the basal layer
Band like dermal lymphocytic infiltrates
Colloid bodies
Max –Joseph spaces
Management of LP
Challenging for both patient and physician
Only minor symptoms or considerable discomfort and disability
Many drugs lack conclusive evidence for efficacy
Oral LP
General measure
Good oral hygiene and regular professional dental care
Offending drugs or dental amalgam, gold- withdrawal and replacement
Topical lidocaine gel or Diphenhydramine for pain relief
Topical steroids
- First line therapy in mucosal LP
- Triamcinolone in orabase
- Clobetasol propionate in ointment or paste
- Corticosteroid lozenges
- Betamethasone mouthwash
- Fluticasone propionate spray
Intralesional injection
Chlorhexidine mouth wash and anticandidal drug therapy
Hydrocortisone vaginal pessary
Systemic Glucocorticoids
For extensive, ulcerative/erosive lesion of oral and vulvovaginal LP
Used alone or in conjunction with topical therapy
Prednisolone 30-80mg/day tapered over 3-6 weeks
Relapse after dose reduction or discontinuation
Retinoids
Topical tretinoin gel for erosive and plaque like lesion – less attractive because of irritation
Isotretinoin gel for nonerosive oral lesion-improves in 2 months-recovers after discontinuation
In conjunction with topical steroid
Acitretin 30mg/day complete remission in 8 weeks
Cyclosporine
Oral – 3-10mg/kg/day in severe ulcerative diseaseTopical – beneficial but not available commercially
Tacrolimus
Effective in erosive mucosal disease-rapid relief from pain and burningMiscellaneous
Griseofulvin – used empirically
Fluconazole, itraconazole – for candidal overgrowth, concomitant use with systemic steroid
Hydroxychloroquine – 200-400mg/d for 6 months – complete healing of oral lesion
Azathioprine, cyclophosphamide
Laser therapy
Surgical excision of persistent ulcer
Cutaneous LP
Topical Glucocorticoids
For limited cutaneous diseasePotent creams is sufficient for symptomatic relief for small area, larger area needs dilution
Intralesional trimcinolone acetonide
(5mg to 10mg/ml) every 4 week – lesion regress within 3-4 monthsHypertrophic LP:-10-20mg/ml
Monitor for atrophy or hypopigmentation
Retinoids :
Acitretin : 30 mg / day for 8 weeks
Tretinoin : 10-30 mg/d
Etretinate : 10-20 mg/d
Photochemotherapy :
PUVA in generalized cutaneous LP
50 mg of Trioxsalen in 150 L of water - 10 min of UVA bath
75 patients – 65% cured ; 15% improved
Immunosuppressive therapy
Cyclosporine: 3-10 mg/kg/d
Azathioprine , mycophenolate mofetil
Ind : recalcitrant LP
Miscellaneous :
Dapsone : 200 mg/d
Hydroxychloroquine : 200-400 mg/d
IFN- α2b
Metronidazole : 500 mg b.d
Cyclophosphomide ,methotrexate
Prognosis :
Unpredictable ; 1-2 yrs
Duration α extent /site/ morphology
L planopilaris : most chronic
Generalised : rapid course
Gen < skin
Relapse : 15 -20 %






I would like to say that this blog really convinced me, you give me best information! Thanks, very good post. It's really interesting... Keep sharing with us such interesting topics…
ReplyDeleteRegards,
Lichen planus pigmentosus specialist